Call: (816) 887 8587 Email: info@unitedmbs.com
At United MBS, we understand that accurate and timely Verification of Benefits (VOB) is the first crucial step in the revenue cycle.
Before any care is delivered, it’s essential to confirm a patient’s insurance eligibility, benefits, deductibles, and coverage details. Our expert team handles this complex process for you; ensuring you have clear, verified information upfront before delivering any medical services.
Start Verification of Benefits VOB and Eligibility EOB Process with United MBS Today
Reliable Verification of Benefits & Eligibility


In 2025, many in the healthcare industry are asking this important question. The answer is simple:
Accurate Eligibility Verification is crucial for maintaining financial health and Avoiding Delays in Reimbursements.
Incorrect or incomplete insurance information can lead to costly claim denials, payment delays, and patient dissatisfaction. Our comprehensive VOB services eliminate the guesswork by providing real-time verification that enables smarter financial and clinical decisions.
Why Is VOB & EOB Important?


Ensuring patient eligibility is key to successful medical billing, helping determine if patients are covered under their healthcare plans.
As a trusted partner, United MBS streamlines Insurance Eligibility Verification Services to save you valuable time. Our services are tailored to practices of all sizes and specialties, ensuring accurate Insurance Eligibility Verification and preventing costly claim denials.
Eligibility and benefits verification helps healthcare providers assess patient coverage before delivering services, minimizing financial risk.
Patient Eligibility Verification Process
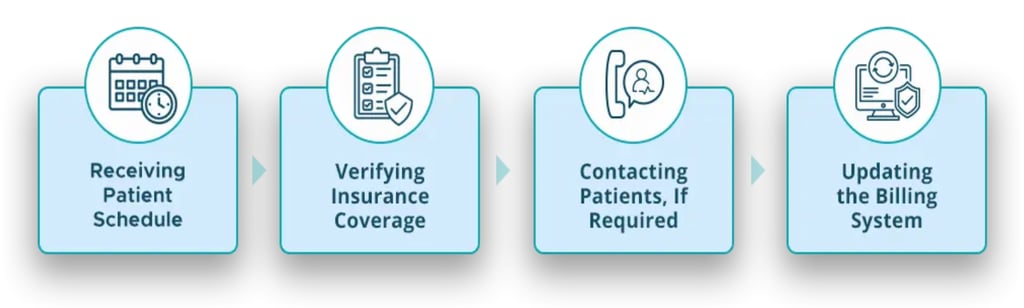

Verify patient insurance coverage & co-pays upfront to avoid any complications and claim denials. Save time and revenues!
What are the consequences of not performing Insurance Eligibility Verification?
Failure to verify insurance eligibility can result in delayed or denied payments, increased costs, and patient dissatisfaction. It also leads to claim denials and collection issues.
How to Verify Insurance Eligibility and Benefits?
Collect patient information, contact the insurance payer, verify benefits, determine patient responsibility, and document all details. Electronic verification tools can expedite this process.
Is authorization required for all medical procedures?
Authorization requirements vary by insurance company. Always check with the payer to determine if a procedure needs prior authorization.
What is the first step in patient eligibility verification?
The first step is collecting relevant patient information, including insurance policy details, to verify coverage and benefits.
Can I verify medical insurance coverage online for free?
Some insurance payers offer free online eligibility verification tools. However, always ensure the accuracy of the information obtained.
Frequently Asked Questions about EOB & VOB


Reach out for
Reliable Medical Billing Services


United MBS delivers accurate, compliant medical billing services nationwide, reducing denials and maximizing revenues for all specialties.
+1-816-887-8587
© 2026. United MBS, All rights reserved.


Quick Links
Services
117 Lexington St, Harrisonville, MO 64701
6226 Grace Marie Dr, Clarksville, MD 21029
Eligibility and Verification Services
Contact Us
424 E, 16th Street, Covington, KY, 41014-1306
